With the winter and flu season approaching, now is a good time to assess the health of pharmacy provision in England and Wales.
To help with this, recent research from Dr Stephen Clark and Dr Andy Newing, published in the Journal of Pharmaceutical Policy and Practice highlights geographical variations in access to community pharmacies.
The problem
Prescribed medication, supplied by community pharmacies is the most common way of treating patients in the NHS. In addition to this NHS prescribing, many pharmacies have the option to offer additional services, a key part of primary care reform in England. Such pharmacies played a key role in administering vaccinations during the Covid-19 pandemic.
The high-profile Darzi report however notes a recent trend in pharmacy closures, with reductions in both opening hours and government funding. As a result, residents of many communities face increasing challenges in accessing pharmacy services.
The background
The flagship Pharmacy First scheme, launched in 2024, enables pharmacists to diagnose and treat seven common conditions without the patient needing to see their own GP.
This strengthens the role of pharmacies in providing primary care, yet pharmacy closures have continued.
However Pharmacists can decide to restrict opening hours or the range of services offered in the face of rising costs.

Pharmacy provision in England and Wales
Pharmacies are private businesses operating under contract to the NHS via the Community Pharmacy Contractual Framework (CPCF). They receive a ‘Single Activity Fee’ for each item dispensed. Many also offer ‘over the counter’ medicines and goods that do not require a prescription.
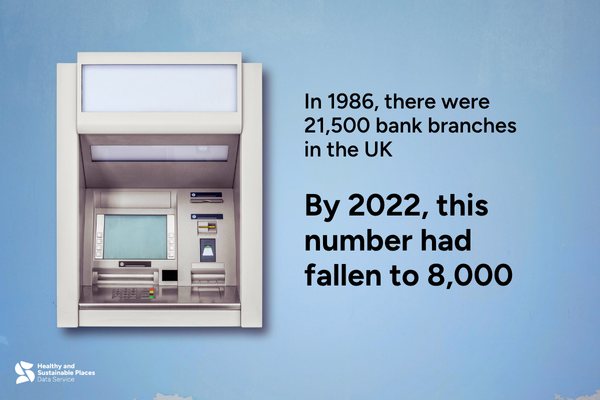
Our analysis reveals that there were 10,924 pharmacies in England and Wales in early-2024, down from 11,507 in mid-2022. There has also been a gradual reduction in opening hours, with only 842 pharmacies open for more than 72 hours a week in early-2024, compared to almost 1,500 in mid-2022.
Our findings agree with industry insights: “The National Pharmacy Association estimates that 7 million hours of pharmacy time has been lost to patients in the last two years, with rural areas particularly impacted as pharmacies have been forced to cut their opening hours or close altogether due to the impact of 40 per cent cuts to funding in the past decade.”

Evidence suggests that the UK has fallen behind other European nations on key metrics of pharmacy provision, such as number of pharmacies per 100,000 people, lagging behind Romania, Turkey, Bulgaria and France. It is clearly important, therefore to understand the impacts of closures on accessibility of the pharmacy network. Whilst some patients use online ‘distance selling pharmacies’, supplying NHS medication direct to patients, usage of these services have declined post-pandemic. Bricks-and-mortar community pharmacies therefore remain the primary means through which prescriptions are fulfilled and are a core part of the neighbourhood-level provision of primary care.
Improving understanding of pharmacy accessibility through research
There are a lack of contemporary studies capturing access to pharmacies in a UK context. Our research uses a measure of accessibility to understand where access to community pharmacies is best and worst, and where the impact of recent closures has been the greatest.
We use pharmacy locations and their opening hours to calculate a neighbourhood level Spatial Accessibility Index (SPAI). Our SPAI captures accessibility of community pharmacies in England and Wales for patients travelling by car. We calculate this measure for every neighbourhood (Lower Super Output Area – LSOA) using the pharmacy network in 2022 and again in 2024.
The SPAI is calculated using a Modified Huff Variable 3 Stage Floating Catchment Area (MHV3SFCA). It accounts for the provision of pharmacies and their opening hours (as a measure of capacity). Neighbourhoods with a higher SPAI will generally have more pharmacies available in close proximity, with longer pharmacy opening hours and a lower overall population ‘competing’ to use those pharmacies.
Our overall SPAI fell by 10% between 2022 and 2024, highlighting the net loss of pharmacy provision and an overall worsening of accessibility of the pharmacy network. We here use our SPAI to understand the geographical inequalities in pharmacy provision and accessibility.
Pharmacy deserts
Prior research noted that nearly 90% of the English population are within a 20 minute walk of a pharmacy, though inequalities between neighbourhoods, especially between urban and rural, have been well documented.
Our analysis confirms these differences in access to pharmacies between urban and rural neighbourhoods, with markedly reduced accessibility for residents in rural locations. However, there is some evidence that rural areas have been impacted less than their urban counterparts in relation to pharmacy cuts between 2022 and 2024, though from a much lower starting point.
| Area Type | SPAI 2022 | SPAI 2024 | Change in SPAI |
| Urban major conurbation | 6.97 | 6.26 | -10% |
| Urban minor conurbation | 6.57 | 5.98 | -9% |
| Urban city and town | 5.48 | 4.83 | -12% |
| Rural town and fringe | 5.31 | 5.08 | -4% |
| Rural village | 0.76 | 0.69 | -8% |
In 2024, the National Pharmacy Association warned of the emergence of ‘pharmacy deserts’ in rural and deprived areas. We adopt the term ‘pharmacy deserts’ to refer to those neighbourhoods with poorest pharmacy provision, as calculated by our SPAI.
The map below shows the 0.1% of LSOAs in England and Wales with the lowest score on our SPAI, in 2022. These we consider to represent pharmacy deserts. These are exclusively in rural or semi-rural areas, with clusters in South West England and mid-Wales.

Regional Case Studies
As well as a national perspective on the location of possible pharmacy deserts, it is possible to explore the situation in various localities. In the accompanying article we did this for the city of Preston in North West England. Here we present three additional case studies.
Leicester (East Midlands)
The city of Leicester is the largest city in the East Midlands and shows a variety of accessibility levels. There is good accessibility to community pharmacies in the city centre and towards the west of the centre. The more rural locations in the north west have comparatively poorer accessibility. The railway line running north to south through the city acts as a barrier, preventing people from using alternative pharmacies either side, though the high provision of pharmacies, especially to the east of the railway line, limits the impact on accessibility scores in many neighbourhoods.
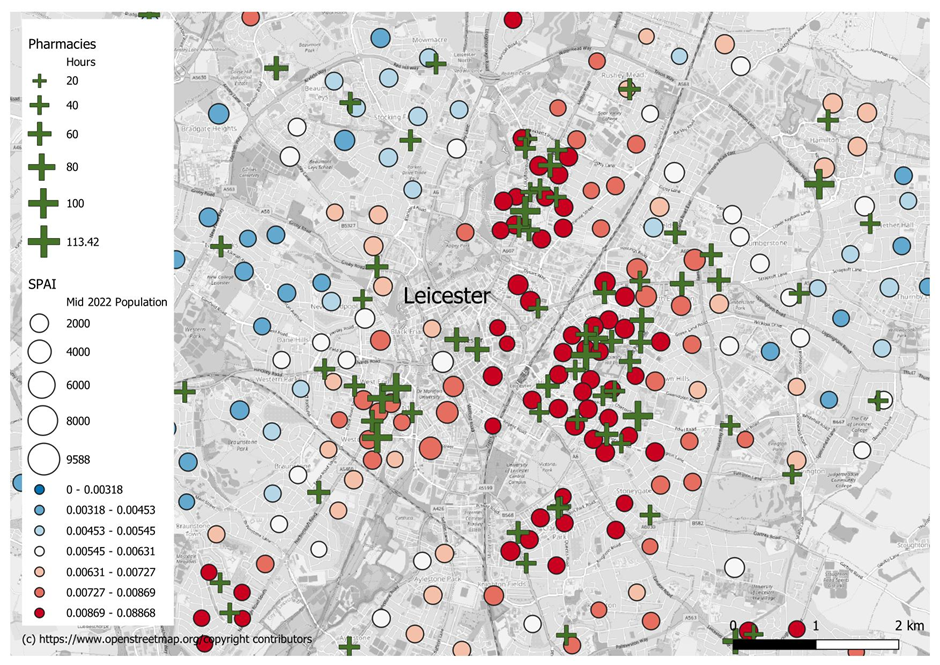
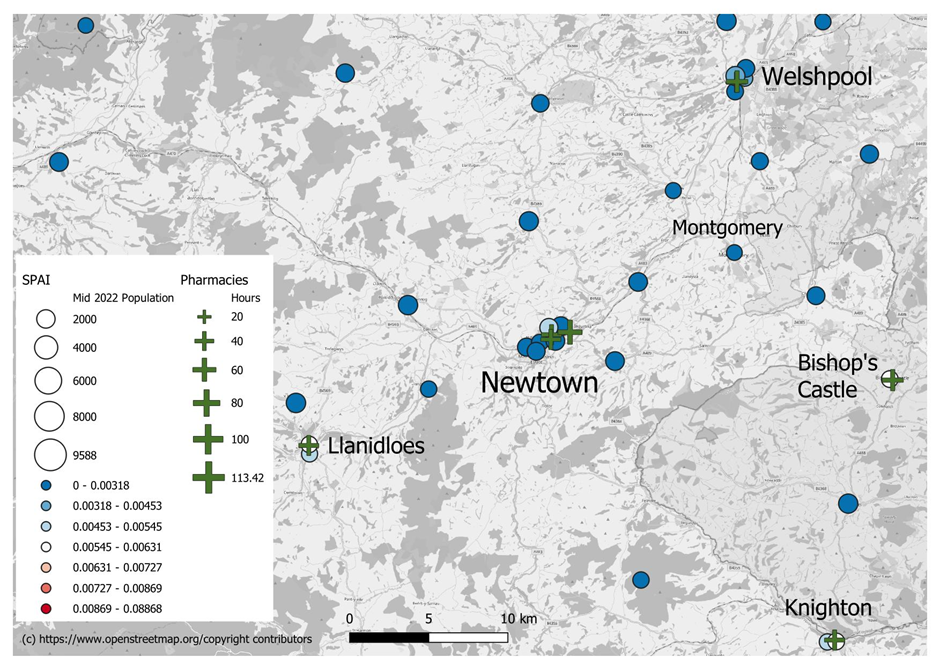
Note that these maps show the location of pharmacies with a green cross, and the size of the cross is proportional to the opening hours of the pharmacy. They also show the demnd (population) as circles, with the size of the circle being proportional to the size of the 2022 mid-year population estimate for that neighbourhood. The colour of the circle also shows which range the SPAI falls in, with blue being neighbourhoods having lower accessibility and red neighbourhoods having higher accessibility.
Torquay, Paignton and Brixham (South West).
These three coastal towns show a variety of levels of accessibility. The accessibility is good in both Torquay and Brixham but poor in Paignton. Paignton has just six pharmacies to serve its population, a similar number to the smaller nearby Brixham community. Torquay has many pharmacies available to its population, and thus has good accessibility.

Newtown (Wales)
Newtown is a town in mid-Wales, located in the narrow river Severn valley. It is served by three pharmacies. However there are a number of smaller villages around Newtown without any pharmacies, thus there is extra demand placed on these three pharmacies in order to serve these wider communities.
Positive care law
Previous research has also highlighted a ‘positive pharmacy care law’, with evidence of better access to pharmacies in many deprived neighbourhoods, where needs may be greatest.
Our findings support the existence of the ‘positive pharmacy care law’, with higher SPAI scores in relatively more deprived areas. Whilst overall accessibility of the pharmacy network has declined within the relatively more deprived neighbourhoods, the rate of change is comparable to other area types.
| Area Type | SPAI 2022 | SPAI 2024 | Change in SPAI |
| Highest Deprivation | 6.96 | 6.19 | -11% |
| High Deprivation | 6.41 | 5.73 | -11% |
| Middle Deprivation | 5.62 | 5.03 | -10% |
| Low Deprivation | 5.26 | 4.72 | -10% |
| Lowest Deprivation | 5.09 | 4.55 | -11% |
Pharmacy closures could widen neighbourhood health inequalities
Pharmacies are an important gateway to the primary health system, located across our communities, promoting self-care and supporting public health. One estimate suggests that they save an average of 95 consultations in every GP surgery each week, thereby reducing pressures elsewhere in the health system.
The positive pharmacy care law evidenced in our work highlights the important role of pharmacies in reducing health inequalities and promoting access to healthcare within these neighbourhoods. Yet, ongoing fears of closures heightens the risk of more neighbourhoods becoming pharmacy deserts.
It is unclear what role pharmacies will play in the government’s 10-year health plan (due for publication Spring 2025), but ongoing uncertainty around the future of funding underpinning Pharmacy First, and for other pharmacy services such as blood pressure monitoring, increase the risk of future pharmacy closures.
Our analysis, reported fully in the accompanying academic paper, highlights the importance of spatial analysis in uncovering geographical inequalities in access to core services such as community pharmacies. Our ongoing work seeks to further improve our SPAI, capturing the full range of services offered by each pharmacy along with a more nuanced measure of pharmacy capacity.
It is also important to understand how patients and customers are using the pharmacy network, including their use of distance selling pharmacies. We are exploring future opportunities that could be afforded by Smart Data Research UK to use transactional smart data to capture (fully anonymised) individual interactions with the pharmacy network as provided by loyalty card, financial and mobility records. These could enable us to build accessibility models that more accurately reflect how individuals use the pharmacy network, especially the choice of pharmacy visited.